Parathyroid Surgery for Hyperparathyroidism (HPT)
-
What are parathyroid glands?
-
What is hyperparathyroidism?
-
How do you treat HPT?
-
Is it possible to detect which parathyroid glands are enlarged before the operation?
-
What happens before the operation?
-
What does the operation involve?
-
Intraoperative PTH assay?
-
Are there any risks to the operation?
-
What are the results of surgery?
What are parathyroid glands?
You have four parathyroid glands, two on each side of the neck which lie against the thyroid gland. The thyroid gland is shaped like a butterfly with a left and a right side (lobe) joined in the middle by a small bridge. In simple terms the parathyroid glands are situated at the four corners of the butterfly’s wings, each the size of a grain of rice. These produce a hormone which controls the level of calcium in the blood; parathyroid hormone (PTH) which controls the level of calcium in the blood. Calcium is an important salt involved in many processes in the body.
What is hyperparathyroidism?
Hyperparathyroidism (HPT) occurs when there is an excess of PTH in the blood. Most of the time (90%) this is due to a non-cancerous growth of one gland, but in a minority (10%) it occurs because more than one gland has become enlarged. Too much PTH leads to too high a level of calcium in the blood and this can cause problems with the bones, the kidneys and produce symptoms including headache, thirst and loss of energy. In the longer-term, a high calcium is harmful to the heart and the kidneys.
How do you treat HPT?
Removal of the enlarged parathyroid glands is currently the only treatment which permanently returns the blood calcium to normal levels. The high success rate and safety of parathyroid surgery justifies an operation in nearly all patients diagnosed with HPT.
Is it possible to detect which parathyroid glands are enlarged before the operation?
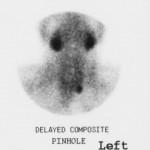
No pre-operative imaging test is as good as an experienced endocrine surgeon. However, there are two special scans which may identify enlarged parathyroid glands before surgery. These are a nuclear medicine and an ultrasound scan of the neck. A combination of these two scans accurately identifies abnormal glands in about 80% of patients. However these scans are unreliable in distinguishing those patients with just one abnormal gland, from the fewer patients with enlargement of two or more glands. Nevertheless the scans provide your surgeon with valuable information prior to the operation, particularly if the abnormal gland is found in a location outside the neck.
What happens before the operation?
You will usually have a pre-assessment to confirm your fitness for a general anaesthetic two weeks before operation and be admitted to hospital on the day of surgery. Pre-operative tests may include a chest X-ray, a heart recording (e.c.g.) and various blood tests.
What does the operation involve?
The surgery is carried out under a general anaesthetic. During your operation the surgeon will attempt to find and remove all abnormal parathyroid gland or glands and identify, inspect the other parathyroid glands. Abnormal glands may not be found at the time of the operation in about one patient in twenty (5%) either because the gland is so small or hidden that it cannot be found or very rarely because the gland lies not in the neck but in the chest. If that is the case you may need another operation at another time to remove it. The blood calcium is measured the morning after surgery and most patients are fit to go home 24h after surgery.
Intraoperative PTH assay
At University Hospital of Wales we have the technology to measure the fall in PTH at the time of the operation. This has two advantages. In situations where the parathyroid tumour has been localised before surgery, only one side of the neck is explored minimizing the time of surgery and the dissection. Knowledge that the PTH has fallen informs the surgeon that the operation has been successful straight away.
Are there any risks to the operation?
Operations on the parathyroid glands are very safe but sometimes there are complications.
Failure to cure: This is uncommon (3%), but is, in fact, the commonest complication! Reasons to fail are either because the surgeon has failed to realise that there is more than one tumour, or the tumour cannot be found.
The Voice: Intimately related to the thyroid gland and so sometimes the parathyroid glands are two nerves, one on each side of the neck. These recurrent laryngeal nerves provide the electricity for the movement of the vocal cords – which generate the voice. Injury to the nerve causes a weak and husky voice. Most injuries are a temporary bruising, with full recovery. However a permanent injury will result in a permanently weak voice. The risk of a permanent injury in parathyroid surgery is less than 1% (one in one hundred).
The Scar: Parathyroid surgery is undertaken through a 3 – 4cm scar that follows the natural creases in the neck. Usually it heals well leaving only a thin line. The stitches that are used dissolve and so there is no need for them to be removed. Application of Vitamin E to the wound greatly improves the cosmetic result.
What are the results of surgery?
The calcium returns to normal in 95% of patients at the first attempt. Rarely the calcium falls to below the normal level and you may experience pins and needles of the hands, lips and feet. The remaining glands will recover their normal function but in the meantime you may require calcium and vitamin D tablets. For patients with four abnormal glands, a subtotal (three and one half) parathyroidectomy is usually undertaken and calcium supplementation may be prolonged.